Introduction
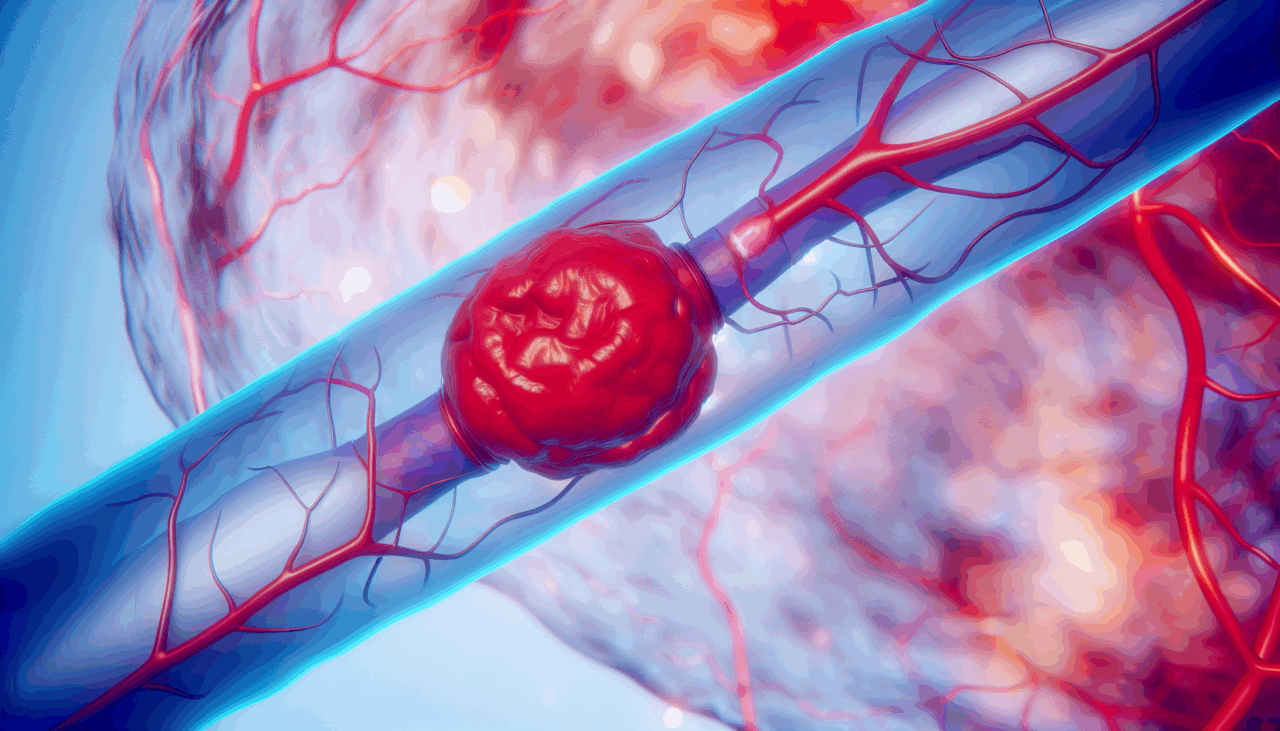
Ischemic stroke is a prevalent and severe neurological condition characterized by high rates of incidence, disability, and mortality, imposing a significant societal and economic burden. The blood-brain barrier (BBB) plays a crucial role in the pathological process of cerebral ischemia. It acts as a specialized structure between the blood and brain tissue, preventing harmful substances from entering the brain, maintaining the stability of the brain’s internal environment, and ensuring normal neuronal function.
Vascular Recanalization and Its Implications
Vascular recanalization is a cornerstone therapeutic strategy for cerebral ischemia. Clinical interventions such as intravenous thrombolysis and mechanical thrombectomy aim to reopen occluded blood vessels, restore blood supply to ischemic brain tissue promptly, and reduce neuronal death. However, while vascular recanalization restores blood flow, it may also lead to ischemia-reperfusion injury, further damaging the BBB and potentially leading to hemorrhagic transformation in severe cases. This complication significantly increases patient disability and mortality rates. Understanding BBB changes following vascular recanalization is crucial for exploring new approaches to protect BBB integrity, reduce its permeability, and lower the risk of hemorrhagic transformation.
The Blood-Brain Barrier: Structure and Function
The BBB is a complex dynamic functional system composed of various cells and molecules, primarily brain microvascular endothelial cells (BMECs), basement membrane, pericytes, and astrocyte endfeet. These components work together to maintain BBB function. BMECs form a tight monolayer structure that restricts the free passage of most substances. Alterations in BBB permeability involve multiple mechanisms, with changes in tight junction proteins and transcytosis playing key roles.
Tight Junction Proteins and BBB Integrity
Tight junction proteins are pivotal in maintaining the integrity of the paracellular pathway at the BBB. Following cerebral ischemia, the expression and cellular distribution of key tight junction proteins such as claudin-5, occludin, and ZO-1 are markedly altered, leading to the disruption of tight junction structure and increased BBB permeability. During ischemia-reperfusion, these proteins are significantly downregulated, and their localization shifts from a continuous linear pattern to fragmented arrangements along the cell membrane, enlarging intercellular gaps and facilitating paracellular leakage into brain tissue.
Transcytosis and BBB Permeability
Under normal conditions, transcytosis across BBB endothelial cells is limited, preserving barrier selectivity. However, cerebral ischemia, particularly upon reperfusion, leads to a pronounced upregulation of transcellular transport mechanisms. Caveolae-mediated transcytosis, in particular, has been implicated in increased BBB permeability after ischemic events, facilitating the vesicular transport of macromolecules such as albumin and immunoglobulins, compromising barrier integrity.
Research Methodology
In this study, 8-9-week-old male C57BL/6J mice were used. Mice were divided into recanalization and non-recanalization groups. The recanalization group underwent middle cerebral artery occlusion and reperfusion 60 minutes later, while the non-recanalization group experienced permanent occlusion. BBB permeability was tested using fluorescence staining, and the expression of tight junction and transcytosis-related proteins was analyzed by western blot.
Results and Findings
The IgG results revealed a significantly larger area of leakage in the recanalization group compared to the non-recanalization group. A consistent trend was observed in the FITC-dextran leakage experiment. After blood flow recanalization, there was a significant reduction in tight junction-related proteins, occludin and ZO-1. Both ischemia and reperfusion caused changes in the ratio of transcytosis-related protein Caveolin-1/MFSD2a, more pronounced in the recanalization group.
Conclusion
Vascular recanalization exacerbates BBB disruption, impairing both paracellular and transcytosis pathways. This finding provides a rationale for exploring new approaches to protect BBB integrity, reduce its permeability, and lower the risk of hemorrhagic transformation. Successful recanalization is only the first step; comprehensive neuroprotection and improved patient outcomes require a multi-target therapeutic strategy that reinforces tight junctions and suppresses pathological transcytosis.
Limitations and Future Directions
The study’s limitations include the exclusive use of male animal models, which precludes generalization to females. Future research should include both sexes to determine the translatability of these mechanisms across populations. Additionally, the study did not investigate claudin-5, a primary transmembrane protein critical for paracellular seal formation, limiting a comprehensive mechanistic understanding of BBB permeability changes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
🔗 **Fuente:** https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1682748/full